Introduction: Building Trust Before Care Begins
In the fast-evolving world of U.S. healthcare, one thing remains constant—trust. Patients trust that their doctors are qualified, insurance companies trust that providers meet compliance standards, and healthcare facilities trust that their staff are credentialed to deliver care.
This crucial process that establishes that trust is known as provider credentialing—a detailed verification procedure that ensures healthcare professionals meet the standards set by regulatory bodies, insurers, and hospitals.
Yet, credentialing is more than just paperwork. It’s the first step toward getting reimbursed, joining insurance networks, and ensuring compliance. That’s why many U.S. healthcare providers now rely on professional credentialing services for providers, offered by trusted partners like 24/7 Medical Billing Services.
What Is Provider Credentialing, and Why Does It Matter?
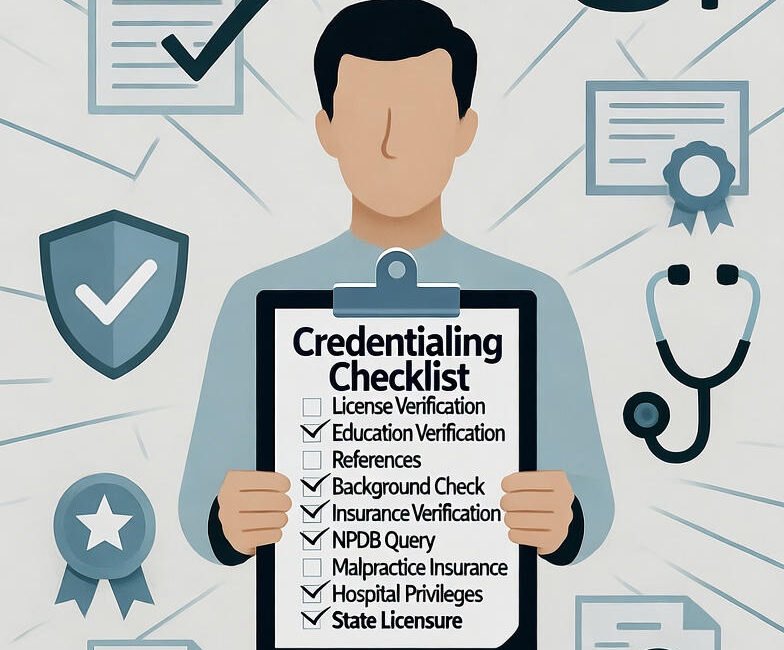
Credentialing involves the thorough verification of a healthcare provider’s qualifications—including their education, training, experience, and licenses.
Before a provider can treat patients under an insurance plan or work in a medical facility, they must be credentialed and enrolled with various payers. This process ensures accuracy, compliance, and patient safety.
Key Steps in Provider Credentialing
Data Collection: Gathering the provider’s personal and professional details, education history, and licenses.
Verification: Validating all credentials with the primary source (schools, licensing boards, etc.).
Payer Enrollment: Submitting and following up on applications with insurance networks.
Ongoing Maintenance: Renewing credentials and revalidating licenses periodically.
Failure in any of these steps can cause delays in payments, claim denials, or even loss of network participation. That’s where expert RCM and credentialing partners step in.
Challenges in Credentialing for U.S. Healthcare Providers
Healthcare providers often underestimate the time and complexity involved in credentialing. Here are a few pain points that many practices face:
Long Processing Times: Payer credentialing can take anywhere from 60 to 120 days or longer.
Complex Paperwork: Each insurance carrier has unique forms and requirements.
Frequent Follow-ups: It takes persistence and coordination to track each application’s progress.
Risk of Denials: Small errors or outdated information can lead to rejected or delayed applications.
Renewal Deadlines: Providers must revalidate credentials regularly to stay active with payers.
These challenges not only strain administrative staff but also delay revenue flow—making professional credentialing services for providers a vital solution.
How Credentialing Services for Providers Simplify the Process
Outsourcing credentialing to experts like 24/7 Medical Billing Services allows healthcare organizations to focus on patient care while the specialists handle compliance and payer communication.
Here’s how professional credentialing services streamline the process:
1. Expert Guidance and Accuracy
Credentialing specialists have deep knowledge of payer requirements and state-specific regulations. They ensure every document and submission is accurate and up-to-date—minimizing errors that lead to delays.
2. Faster Turnaround Times
With an experienced team managing follow-ups and documentation, providers get credentialed faster, reducing downtime and helping them start seeing patients sooner.
3. Complete Compliance Management
Credentialing partners maintain detailed compliance records, ensuring all licenses and certifications stay active—crucial for audits and legal protection.
4. Continuous Monitoring and Revalidation
Professional services track re-credentialing dates, submit updates, and ensure uninterrupted payer participation.
5. Seamless Integration with RCM
When combined with Revenue Cycle Management (RCM) and medical billing outsourcing, credentialing becomes part of a unified financial ecosystem—improving both compliance and cash flow.
The Business Impact: Why Credentialing Matters Beyond Compliance
Credentialing isn’t just about meeting regulatory requirements—it directly impacts the financial health of a medical practice.
Let’s explore how:
✅ Faster Reimbursements: Properly credentialed providers face fewer claim denials and quicker payments.
✅ Expanded Patient Base: Joining more payer networks increases the number of insured patients a provider can serve.
✅ Stronger Reputation: Verified credentials enhance patient trust and improve hospital affiliations.
✅ Reduced Administrative Burden: Outsourcing frees up internal staff to focus on operations and patient engagement.
✅ Improved Revenue Cycle: Credentialing accuracy reduces billing errors, contributing to a healthier revenue flow.
Why Choose 24/7 Medical Billing Services for Credentialing?
24/7 Medical Billing Services is one of the leading U.S.-based healthcare outsourcing partners providing end-to-end medical billing, RCM, and credentialing solutions.
Here’s what makes them a trusted choice:
Certified Credentialing Experts: Skilled professionals experienced with all major payers, including Medicare, Medicaid, and commercial insurers.
Transparent Process: Regular updates and detailed reports keep providers informed of application status.
Nationwide Coverage: Expertise across all U.S. states and specialties.
Technology-Driven Systems: Advanced software tools ensure accuracy and real-time tracking.
Comprehensive RCM Integration: From credentialing to claims submission and denial management—all handled seamlessly under one roof.
By partnering with 24/7 Medical Billing Services, providers can rest assured their credentialing process is handled with precision and compliance.
Best Practices for Smooth Credentialing
If you’re a healthcare provider or practice manager, follow these tips to make your credentialing process more efficient:
Keep copies of all updated licenses and certifications in one place.
Start credentialing early—especially when onboarding new physicians.
Ensure accurate NPI (National Provider Identifier) and Tax ID details.
Track re-credentialing timelines and renew before expiration.
Partner with a reliable credentialing service provider to manage applications proactively.
Conclusion: Credentialing—The First Step to Financial and Professional Success
Credentialing is not just a compliance requirement; it’s the foundation of trust and revenue in the U.S. healthcare system. Without proper credentialing, even the most skilled providers can face delayed payments and network ineligibility.
By leveraging credentialing services for providers from experienced companies like 24/7 Medical Billing Services, healthcare organizations can ensure faster approvals, accurate documentation, and smoother revenue cycles.
Whether you’re a small clinic or a large hospital, outsourcing credentialing allows your team to focus on what truly matters—delivering quality patient care.

